CONTENTS:
- Experiences of Adolescents and Young Adults (AYAS) with primary Immune Thrombocytopenia (ITP)
- Watchful Waiting: Read about this treatment approach, mechanism of action, benefits, and side effects
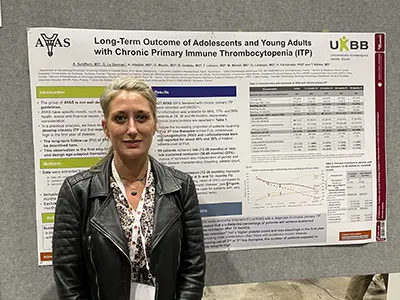
Experiences of Adolescents and Young Adults (AYAS) with primary Immune Thrombocytopenia (ITP)
Currently, ITP is defined in only two age categories:
1. Pediatric ITP, affecting children up to approximately 21 years of age, is often described as a self-limiting disorder (meaning it usually resolves quickly) that causes a low platelet count (thrombocytopenia) usually with sudden onset (acute) and often following a viral infection.
2. Adult ITP, often described as a long-term (chronic) disease that does not resolve quickly and has more of a slow onset (insidious) with increased morbidity and mortality.
Management principles for pediatric and adult ITP consist of different treatment protocols and practice guidelines. Since AYAS are by nature an active group of patients, going through unique hormonal, behavioral, and social changes as they begin their transition to adulthood, understanding how ITP presents and evolves in this particular age group is an important first step to better managing the disease.
Study Detail:
Patient data were collected from three large ITP patient registries (databases of patient-reported medical history used to help better understand the natural history of a disease), including the PARC-ITP (international) registry, the CARMEN-France registry, and OBS CEREVANCE (France), which is a national registry for the follow-up of children with severe autoimmune cytopenia. Patients with secondary or misdiagnosed ITP and pregnant women were excluded from participating.
The following definitions were applied to the study:
- Chronic disease – defined as having a platelet count below 100,000 μL (per microliter of blood) or ongoing treatment one year after diagnosis or a relapse at a later follow-up.
- Remission – defined as a platelet count greater than 100,000.
- Sustained remission – defined as a platelet count of 100,000 beyond the one-year mark without treatment for at least 6 months.
- Late remission – defined as achieving a platelet count above 100,000 anywhere between 12-36 months, while “very late” remission was defined as achieving a platelet count above 100,000 between 36-48 months after diagnosis.
Two separate parts of this study were conducted.
Part one: The Newly Diagnosed AYAS Experience
A total of 656 AYAS (61% female) with primary ITP were included in the first part of the study, and a total of 428 AYAS (64% female) who went on to develop chronic ITP were included in the study. The median age (middle of the age range) of participating AYAS was 15.
Platelet count at first presentation was very low (median 12,000), however, 109 patients presented without bleeding symptoms. Apart from gynecological bleeding, females and males had similar bleeding and half of all patients developed chronic ITP. The chance of remission was higher in patients who, at diagnosis, had a very low platelet count (less than 20,000), especially, if these participants received corticosteroids and/or intravenous immunoglobulins (IVIG) compared to those who did not receive any treatment in the first four weeks following their diagnosis.
There were small differences in the subgroup of adolescents who were between the ages of 12-18 compared to young adults between the ages of 18-25 years. The 12-18-year-old group experienced more moderate thrombocytopenia at diagnosis and less bleeding at all follow-ups compared to the 18-25-year-old group.
Part two: Long-Term Follow-up with AYAS who have Chronic ITP
A total of 428 AYAS with chronic primary ITP were included in the second part of the study. The initial median platelet count at the 24-month follow-up was 15,000. Follow up information was available for 88% at 24 months, 77% at 36 months, and 59% at 48 months. There were 74 patients (19%) who reported no bleeding at diagnosis. Overall, seven patients (1.6%) reported intracranial hemorrhage; three at the time of diagnosis, three within the first six months, and one between 12-24 months.
Patients with sustained chronic disease had a median platelet count of 55,000 at 24 months and 62,000 at 48 months follow up. About half needed treatment during the follow-up. The number of patients who experienced a bleeding event and the location of such a bleeding event was similar across all in this subgroup during the follow ups, with 70% suffering "wet bleeding" (blood blisters in mucosal lining such as in the mouth). The proportion of patients receiving second- or third-line therapies increased with time. However, IVIG and corticosteroids were still reported for about 40% and 30% of treated patients beyond 12 months.
Among those who maintained a sustained chronic disease, 23% showed late or very late remission, and 15% had unknown remission status. They found no differences in symptoms experienced at the time of initial disease presentation between patients with late/very late remission versus patients with sustained chronic disease. However, over time, the AYAS who experienced a late remission displayed less bleeding, higher platelet counts, and needed IVIG less often at six and 12 months compared to AYAS with sustained chronic disease.
In total, 11 patients were diagnosed with secondary ITP after 12 months, including: two with common variable immunodeficiency (CVID), four with Evans syndrome, and five patients with systemic lupus erythematosus (lupus).
The rate of chronic disease was 50% at the one-year mark, unlike what is typically seen in pediatric ITP, however, remission thereafter was still achievable. Remission within 1 year appeared to be associated with earlier administration of treatment; this was not the case for patients with late/very late remission. However, AYAS with late remission had a less severe disease course in the first year of disease (excluding initial presentation) compared to those with sustained chronic disease. Study results also highlighted that AYAS are mainly treated with corticosteroids for the first year and widely throughout the observation period.
Dr. Schifferli’s study highlights the importance of adapting medical care for AYAS, rather than treating them simply as pediatric patients, and could serve as a basis for future studies to establish better diagnostic and therapeutic strategies in AYAS with ITP. Future studies could focus on: (1) accepting ITP of AYAS as a distinct entity from pediatric and adult ITP; (2) adopting treatment endpoints that reduce the rate of chronic disease; and (3) curbing the use of corticosteroids beyond the initial management.
Watchful Waiting
Read about this treatment approach, mechanism of action, benefits, and side effects.
